- Frequent urination, especially at night
- Weak or intermittent urine stream
- Sudden urges to urinate
- Incomplete bladder emptying
Benign Prostatic Hyperplasia (BPH), or prostate enlargement, affects millions of men as they age. The symptoms—frequent nighttime urination, weak flow, urgency—can be more than just an inconvenience. At Endovascular Consultants of Delaware, we offer Prostate Artery Embolization (PAE), a minimally invasive solution that treats the problem without the risks of surgery.
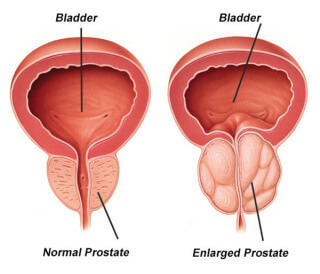
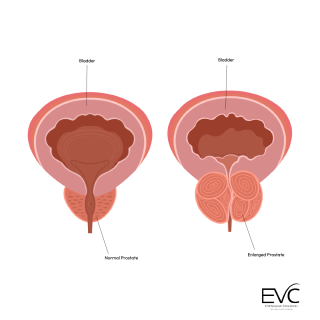
As men age, hormonal changes can cause the prostate to grow. That growth can compress the urethra and affect urination.
BPH isn’t life-threatening, but it can seriously affect your quality of life.
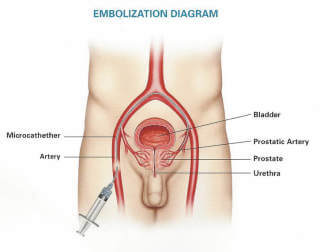
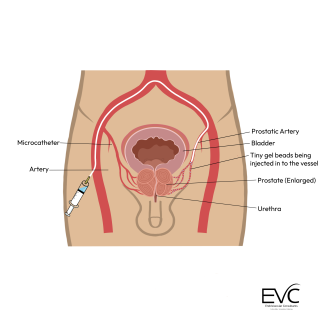
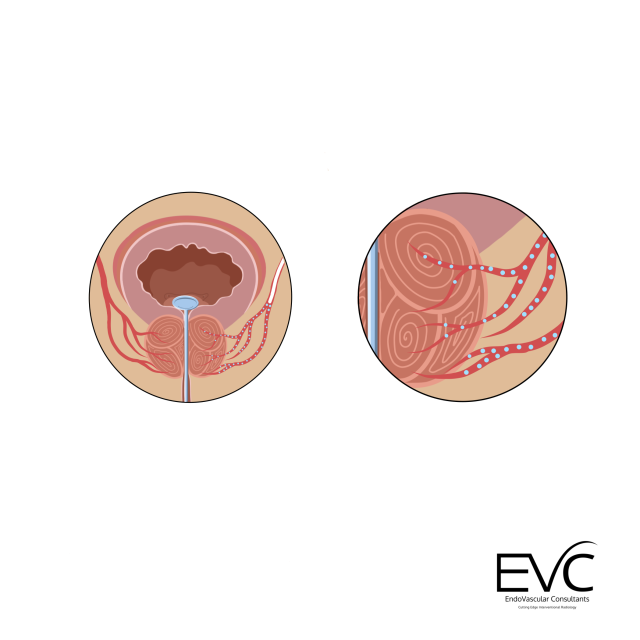
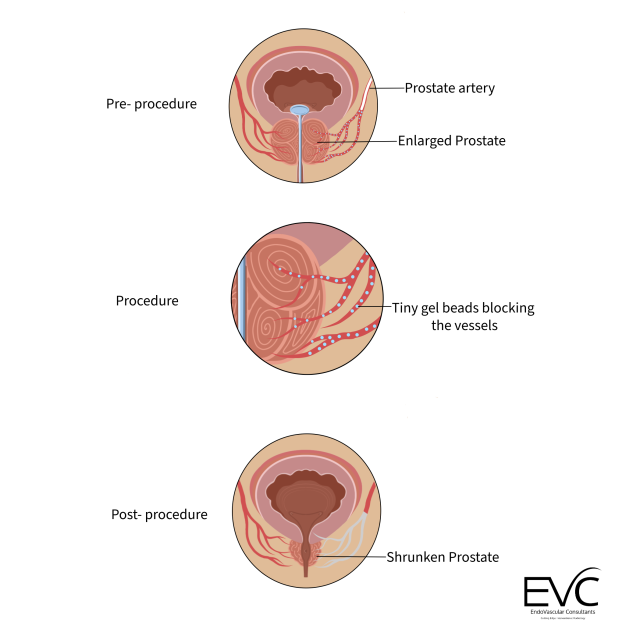
PAE is a non-surgical outpatient procedure that shrinks the prostate by cutting off its blood supply.
Most patients go home the same day and see relief within days to weeks.
Compared to traditional treatments like TURP (Transurethral Resection of the Prostate), PAE offers:

You’re not just choosing a procedure—you’re choosing a team that prioritizes your long-term health and comfort.
You may not need traditional surgery. Let’s talk about what’s possible.
PAE is performed by interventional radiologists—specialists in minimally invasive, image-guided treatments.
You may not need traditional surgery. Let’s talk about what’s possible.

Dr. Mark J. Garcia is a board-certified, world-renowned interventional radiologist with over 25 years of experience. He has held leadership positions across some of the nation’s top vascular centers and medical device companies. Known for his pioneering work in minimally invasive treatments, Dr. Garcia is committed to improving outcomes for every patient he meets.
You don't have to live like this. Let's explore your options together.